Low Level Narrow Band Red Light Treatment of Acne Vulgaris
Introduction
The purpose of this study was to evaluate, by a prospective clinical trial, the therapeutic effect of LLRL on the inflammatory lesions of Acne Vulgaris, and to establish the optimal duration and mode of illumination.
By Avikam Harel M.D.;* Esther 0 Grunis, M.A.; Rina Levran M.D.; and Gideon Earon M.D
Methods
An emitter of LLRL (BioBeam 660) was chosen for the treatment due to its low cost, convenient size, and safety. Its healing properties have been effective in treating wounds such as diabetic ulcers, bed sores, venous ulcers, and post-operative wounds (9). The device may be operated in two modes: continuous wave (CW), which has a maximum power density of 15 mw/cm2 with 18 mw of power at focus; and pulse wave (PW), which has a greater peak power at focus (75 mw) with only half the average power (7.5 mw) (Table 11).
Patients were instructed by the staff and performed treatments at home. Affected areas were Illuminated from a distance of 2 em determined by a plastic ring (diameter 4 em) fitted to the device and held touching the face. Protective goggles were worn to avoid exposure to the eyes.
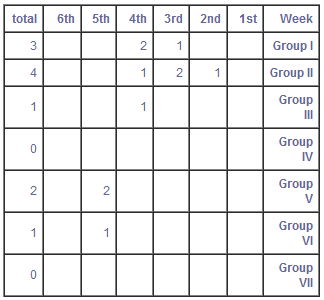
Patients were divided into 5 groups according to the duration and mode of illumination (Table Ill). Eight patients participated in each group except Group V which had five. Patients in Groups 1, 11, and III, applied the device to the affected area twice a day, set to modes CW and PW consecutively, for 1.5, M, and 4 minutes respectively. The 1.5, 2.5 and 4 minutes correspond to a total treatment time of the CW and PW modes used together for 3, 5, and 8 minutes respectively. It became evident that longer exposure to the CW mode provided greater improvement. Therefore, Groups IV and V used only the CW mode for 6 and 8 minutes respectively on each affected area.
Two more groups of patients combined LLRL with medication to determine whether it could enhance the therapeutic effects of exposure to LLRL. One group was treated with contraceptive pills containing cyproterone acetate 2 mg and ethinylestradiol 0.035 mg (Diane-35 Schering Germany), and the other with minocycline 50mg (Minocin, Lederle) twice a day.
The results of eleven patients, mostly from Groups 1 and II who did not complete the 6 weeks of treatment were included in the study up to the time they stopped treatment.
Statistical Methods
The effectiveness of the treatment was measured by the change in the Burton Scale from the pre-treatment level. (A negative value implies worsening of the clinical feature).
Differences between groups were analyzed using Anova and Tukey's method for pairurse comparisons. They were supplemented by the Kruskal-Wallis test where appropriate.
Results
The effectiveness of the 6-minute treatments alone and combined with medication is presented in Figure 1. All three versions exhibit continuous improvement as treatment progressed. By the end of the sixth week, the mean (±SE) improvement achieved by illumination was 1.92 (±.2) change on the Burton scale, with minocin 2.6 (±.2) and with Diane-35, .7 (±.3)
The differences between the three groups are statistically significant: p .001 using Kruskal-Wallis test when judged together. The difference between illumination alone and the minocin group is not significant, while the differences of these two groups to the Diane-35 group are significant (p .05 using Tukey's method). The differences between the three groups presented in Figure 1 were already significant by the third week (p .012). Note that the rate of improvement was the slowest when illumination was supplemented by Diane-35, and fastest when supplemented by minocin. No significant differences were noted between the 6- and 8-minute groups. There is no statistical analysis available for those patients who dropped out due to lack of compliance.
The effectiveness of the illumination at lower duration is presented in Figure 2. The trends show enhanced effectiveness with Increased duration. The full analysis of this data Is not feasible because of the large percentage of subjects who dropped out during the study. The rate of drop-cuts (Table IV) increased when the therapeutic effect was not evident (Groups I,II) and when the illumination period was too long (Group V).
We do use statistical analysis of the third week where only one subject was missing. For the 1.5 minute group, there was a mean "improvement" of -.5; the 2112 minute group -A; and the 4 minute group, +.25. These differences, though compatible with the general trend, were not statistically significant (P= .137). They are all lower than the .44 mean improvement for the 6 minute group for week 3.
Discussion
As an emitter of non-coherent narrow band red light, we used a safe, low-cost device (BioBeam 660) that is widely used in our clinics to treat various wounds such as bed sores, diabetic ulcers, venous ulcers and post-operative wounds. The instrument used deserves special attention. Most of the Low-level laser instruments deliver an energy of 20 mw concentrated in an area of a few square millimeters and result in a power density of 500 to 2000 mw/cm2 (13, 14). The BioBeam 660, however, has a power density of only 15 mwIcm2 i.e., it does not exceed 1/3 the power density of sunlight at noon (approximately 60 mw/cm2). This difference in favor of the BioBeam 660 provides an added safety dimension for the patient.
The aim of the study was twofold: to evaluate the effect of narrow band red light on inflammatory conditions such as Acne Vulgaris, and to establish criteria for the optimal use of red light on such conditions.
Five groups of patients were studied using specified mode and duration of LLRL treatment. Two more groups were examined combining LLRL treatment with medication. We noted less improvement with shorter exposure, and heightened results with increased use of the CW mode. However, when we compared 6-minute- and 8-minute durations of exposure to the CW mode, we noted no significant difference In results, but a marked decrease in compliance. Regarding the mode of treatment, combining PW and CW modes, as was done in Groups I, Il, and III, did not change the course of the treatment which was influenced only by the amount of time spent employing the CW mode. We thus concluded that the optimal time of treatment was 6 minutes twice a day on up to three affected areas using the CW mode.
Two other groups using combined LLRL and medication were tested. One group was treated with Diane-35, the other with minocyclin 50 rag twice a day. The group using Diane-35 showed an initial worsening in the condition, a characteristic of this treatment. Usually there is a two-month period before definite improvement is noticed, however, by combining Diane-35 with BioBeam, we saw signs of improvement as early as one month after initiating treatment.
When we used BioBeam with minacycline, we saw a faster improvement but the quality of the improvement was the same.
We do conclude that LLRL alone or together with minacycline is a safe and effective treatment to be considered among the treatments of Acne Vulgaris.
Figure 1:
LLRL illumination effect on Acne Vulgaris patients, alone, and with medication.
Figure 2:
LLRL illumination effect on Acne Vulgaris patients as a function of illumination time.
TABLE 1 - Acne Grading According to Burton Scale
TABLE II - Light Emitter Specification
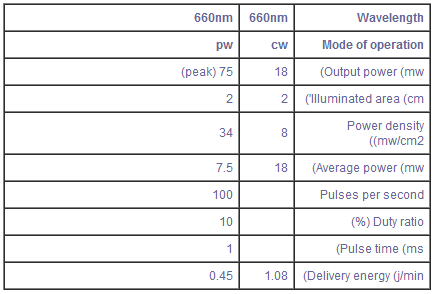
cw= continuous wave / pw= pulse wave
TABLE III - Groups of Patients
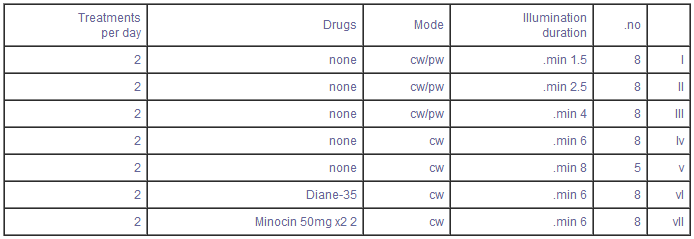
TABLE IV - Rate of Drop-out of Patients from Study
Pediatric Dermatology Outpatient Clinic, Dana Pediatric Medical Center, lchilov Hospital, Tel-Aviv, Israel.
Department of Public Health, Tel-Aviv Municipality.
REFERENCES
1. Mester, E., et. al. Effect of laser rays on wound healing. Am. J. Surg. 1971; 122: 532-535.
2. Calderhead, Glen R. Review of the Biostimulation Session of the 11th Meeting of the American Society for Laser Medicine and Surgery (ASLMS). Lasers in Surgery and Medicine Supplement 3, 1991.
3. Mester, E, et. al. (1985). The biomedical effects of laser application. Lasers in Surgery and Medicine 5, 31-39.
4. Mester, A.F. and Mester, A.R. (1988). Scientific background of laser biostimulation. Laser 1 (1) 23.
5. Karu, T.I. (1988). Molecular mechanisms of the therapeutic effect of low-intensity laser irradiation. Lasers in Life Sciences. 2 (1), 53-74.
6. Sasanov, A.M. et. al. Low-intensity non-coherent red light in the comprehensive treatment of gastroduodenal ulcers. Soy. Med. 12, 42.
7. Abergal, R.P. (1987). Biostimulation of wound healing by lasers; experimental approaches in animal models and fibroblast cultures. Journal of Dermatology and Surgical Oncology 13, 127.
8. Burton J., et. al. The Prevalence of Acne Vulgaris in Adolescence. Dr. J. Derm. 119: 85, 1971.
9. Iusim, M, et. al. Evaluation of the Degree of Effectiveness of BioBeam (Low Level Narrow Band Light) on the Treatment of Skin Ulcers and Delayed Post-Operative Wound Healing. Accepted for publication in Orthopaedics, 1992.
10. Karu, T.l., (1987). Photobiological Fundamentals of lowpower laser therapy. Journal of Quantum Electronics 10, 23.
11. Young, S. et. al. Macrophage Responsiveness to Light Therapy. Lasers in Surgery and Medicine. 9: 497-505 (1989).
12. Young, S. et. al. Effect of light on Calcium Uptake by Macrophages. Original Articles. Lasers in Surgery and Medicine. Supplement 1991 by John Wiley & Sons Ltd.
13. King, P.R. (1989) Low level laser therapy: a review. Lasers in Medical Science 4, 141-150.
14. Rochkind, S. et. al. Systemic Effects of Low-Power Laser Irradiation on the Peripheral and Central Nervous System, Cutaneous Wounds, and Burns. Lasers in Surgery and Medicine 9; 174-182. (1989).
Grade 0 Total absence of lesions
Grade I Sub Clinical Acne-
few comedons visible only in close examination
Grade II Comedonal Acne-
comedons with slight inflammation
Grade III Mild Acne-
inflamed papules with erythema
Grade IV Moderate Acne-
many inflamed papules and pustules
Grade V Severe Nodular Acne-
inflamed papules and pustules with several deep modular lesions
Grade VI Severe Cystic Acne-
many nodular cystic lesions with scarring.
Karu, in her study dealing with the bio-stimulation effect of laser irradiation, suggests that coherence was not always essential for bio-stimulation (10). In effect, in vitro irradiation of macrophage cell culture with non-coherent light at specific wavelengths has been proven to modify their ability to affect fibroblast proliferation (11). The type and degree of modification was found to be dependent upon the wavelengths used. Irradiation with non-coherent light at a wavelength of 660 nm has been shown to produce the maximum stimulatory effect on fibroblast proliferation. It was proposed that non-coherent light may affect macrophage behavior in part via their effect on the permeability of the cell membrane to calcium ions (12). In fact, calcium intake was also shown to be wavelength, dependent and 660 nm was the most effective of the wavelengths tested.
Fifty-three patients, age 14 to 28 years, suffering from Acne Vulgaris (grades 2 to 5 according to Burton scale) (8), were selected for this study (Table 1). The patients were in good physical condition with no endocrine, metabolic, or immunological disorders. Medical evaluation at the beginning of the study and once a week thereafter was carried out by two members of the medical team separately.
The bio-stimulating effects of low level laser irradiation have arroused much interest since the pioneering work of Mester in the early 1970's (1), and were proven in clinical as well as in vitro studies (2),(3),(4),(5). However, It has been shown that at least some of these biological effects can be achieved by exposure to non-coherent low-level red light (6). In fact, macrophages exposed to 660 nm low-level wavelengths release factors which stimulate fibroblast proliferation and mediators of wound repair and inflammatory process healing (7),(11).
Phototherapy treatment using low intensity visible red light (laser) for wound healing is well known. However, its worldwide use is prohibitively expensive and requires a clinical setting. Using a handy, safe and inexpensive non-coherent low level narrow band red light device (LLRL), we performed a prospective clinical trial on 53 patients suffering from Acne Vulgaris. The patients were divided into five groups according to duration and mode of treatment. Two more groups were treated combining phototherapy with medication, The results, following six weeks of LLRL treatment, showed a significant improvement in the group treated twice a day for six minutes by continuous wave (CW). The time reaction to the LLRL treatment was shortened by adding Minocycline (Minocin Lederle) 50 mg twice a day. According to these results, LLRL alone or together with minacycline should be considered a valid and effective treatment for Acne Vulgaris.